We accept all traditional dental insurance plans that allow you to choose your own dentist and dictate your own treatment. We are also in-network preferred providers for many plans. The following are just some of the companies that we work with:


Dental networks are not actual insurance companies, but lease access to dentists to insurance companies, like Aetna, Cigna, Metlife, etc. You should contact your employer or insurance company to determine your eligibility and benefits.
Insurance
If you have dental insurance that is provided by your or your family member's employer, your dental benefits and eligibility for that insurance are determined by your employer and your dental insurance company. Dentists do not determine your benefits or eligibility. Most individual insurance plans that you obtain outside of an employer are generally the most limited with the least amount of benefit and highest premiums. If you have a good individual plan, please let us know, as we have other patients who would be interested in it.
No insurance plan pays 100% of everything. In most cases, insurance companies attempt to pay the least amount possible within their contractual agreement with you (don't forget, they are in the business to make money). Every plan has its' own particular benefits and limitations. You should contact your employers' benefit coordinator or your dental insurance representative for information regarding your plan. If you would like to know more about your plan, or need help deciphering your plans information, please call us, and we will be happy to help you.
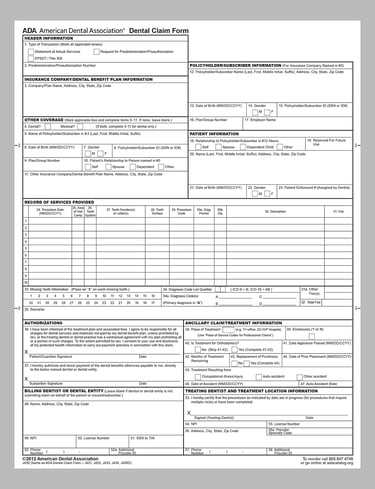
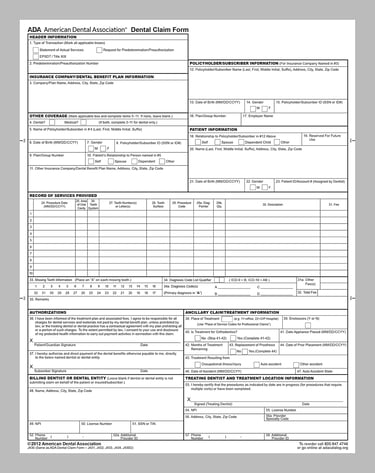
As a courtesy to our patients, we will complete your insurance claim forms for you and submit them to your insurance carrier on your behalf. Please make sure you provide us with your current insurance carrier and employer information as well as your current home address and insurance identification number, as this information must be entered on the insurance claim form.
Dental Insurance Terms
HMO/DMO/DHMO - Dental Health Maintenance Organization. Often the cheapest, but the most restrictive plans. They usually require you to see an in-network provider on a very short list, and will pay nothing if you go outside of that list. They may also provide less incentive for dentists to provide the best or most timely care.
PPO - Preferred Provider Organization. Usually mid-cost plans and the most common. They may or may not offer some incentive for patients to see an in-network dentist, but usually will allow patients to see any provider they want.
Indemnity or Fee for Service (FFS) - Traditional insurance plans that allow you to go anywhere for service. Possibly the most expensive, but the least restrictive.
Benefit Year - Usually a calendar year (January 1 to December 31). Sometimes the year may be based on a company's fiscal year or enrollment period, but generally it's still 12 months long.
Plan Maximum - The total amount that a plan will pay in a benefit year.
Deductible - The amount a patient has to pay before their insurance company pays anything. Usually a single amount for the entire benefit year. Often does not apply to preventative services.
Preventative Services - Exams, basic cleanings, and usually x-rays.
Basic Services - Typically includes fillings, basic extractions, deep cleanings, and root canals.
Major Services - Usually includes crowns, bridges, dentures, complicated surgical procedures, and implants.
Cosmetic Services - Any procedure performed solely for esthetic purposes. Typically this includes whitening, and veneers or crowns where there's no obvious damage to the tooth.